Quick facts about knee gout
- Gout in the knee affects approximately 5% of all gout cases
- Knee gout can cause pain levels comparable to childbirth during acute attacks
- With proper treatment, most knee gout attacks resolve within 3-10 days
- Untreated knee gout can lead to permanent joint damage
- Dietary changes can reduce knee gout attacks by up to 40%
What is gout in the knee?
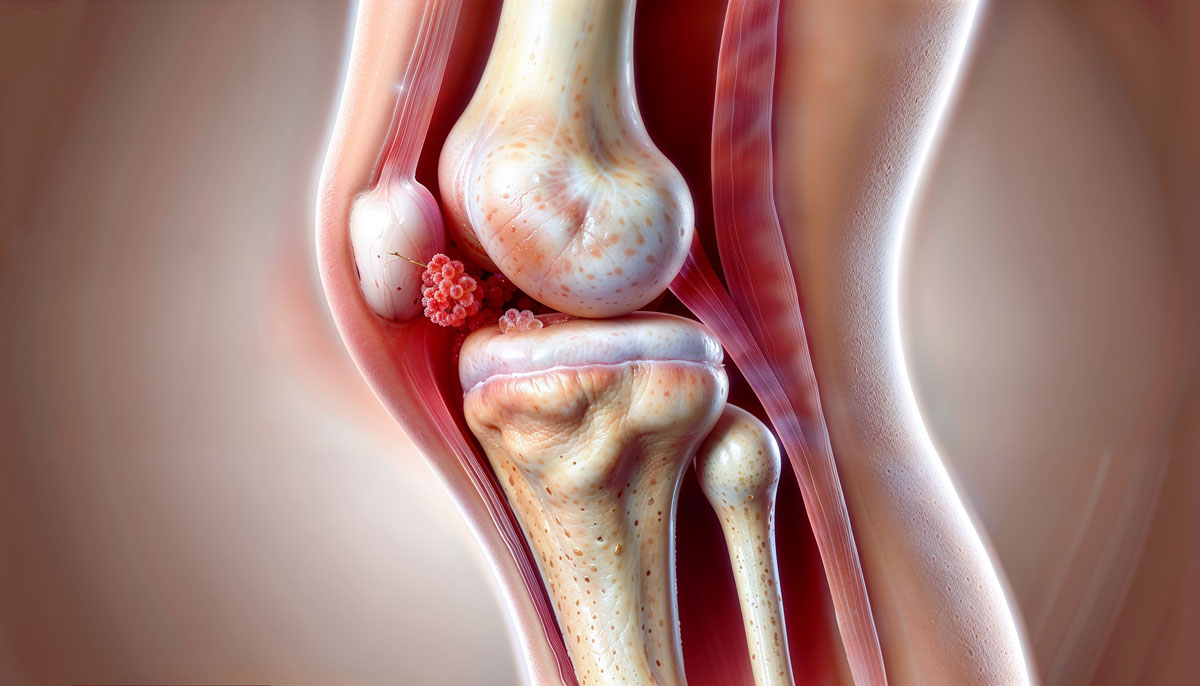
Gout is a painful type of inflammatory arthritis caused by the buildup of uric acid crystals in the joints. While it commonly affects the big toe, gout can also target other joints, including the knee. When gout affects the knee, it can lead to sudden and severe pain that interferes with daily activities.
Knee gout occurs when excess uric acid in the bloodstream forms needle-like crystals that deposit in the knee joint. These crystals trigger an intense inflammatory response, causing the characteristic pain, swelling, and redness associated with gout attacks.
Can gout affect the knee?
Yes, gout can definitely affect the knee. While the big toe (known medically as the first metatarsophalangeal joint) is the most common site for gout, the knee is actually the second most frequently affected joint, accounting for about 5-10% of all gout cases.
The knee joint is particularly susceptible to gout attacks because:
- It’s a weight-bearing joint subject to regular stress
- It has a relatively cool temperature compared to core body temperature
- It contains synovial fluid where uric acid crystals can easily form
- It has a large joint space where crystals can accumulate
Many people are surprised to learn that gout can affect the knee, often mistaking their symptoms for other knee conditions. However, the distinctive nature of gout attacks—characterized by their sudden onset and intense pain—helps distinguish knee gout from other conditions.
Symptoms of gout in the knee
Gout in the knee often strikes without warning, with symptoms that can develop quickly and become quite intense. Recognizing these symptoms early can help you seek appropriate treatment faster.
Primary symptoms
- Severe pain: Gout flare-ups in the knee cause sharp, intense pain, usually starting in the middle of the night or early morning. The pain may be so severe that even light contact with the knee can be unbearable.
- Swelling and redness: The affected knee joint often swells up, becoming visibly larger than the other knee. Redness and warmth in the area are common as well.
- Limited mobility: Moving the knee can become difficult or impossible due to pain and stiffness. This makes even simple tasks, like walking or climbing stairs, challenging.
- Sudden flare-ups: Gout attacks tend to come on suddenly and can last for days or even weeks if left untreated.
Early warning signs
Before a full-blown gout attack, you might experience these early warning signs:
- Mild itching or burning sensation in the knee
- Slight stiffness in the joint
- A feeling of warmth in the knee
- Minor discomfort when bending or straightening the leg
- Slight swelling that might be barely noticeable
Symptom progression timeline
Gout pain scale
- Level 1-3: Mild discomfort, awareness of the knee joint
- Level 4-6: Moderate pain, difficulty walking normally, noticeable swelling
- Level 7-8: Severe pain, significantly limited mobility, pronounced swelling and redness
- Level 9-10: Excruciating pain, complete inability to bear weight, extreme swelling and tenderness
Atypical presentations
While the symptoms above are typical, gout in the knee can sometimes present differently:
- Chronic knee gout: Instead of acute attacks, some people experience persistent low-grade pain and swelling
- Polyarticular gout: The knee may be affected alongside other joints simultaneously
- Tophaceous gout: In advanced cases, visible lumps (tophi) may form around the knee joint
- Migratory gout: Pain that starts in the knee but moves to other joints
If you’re experiencing any of these symptoms, especially alongside joint pain in other areas, it could be a sign of gout in the knee.
Causes of gout in the knee
Gout is caused by a buildup of uric acid in the bloodstream, which forms needle-like crystals that settle in the joints, leading to inflammation and pain. But what causes uric acid to rise? Here are the key factors:
1. Diet rich in purines
Purines are natural substances found in certain foods that break down into uric acid. A diet high in purine-rich foods can lead to elevated uric acid levels, increasing your risk of gout. High-purine foods include:
- Red meats (especially organ meats like liver)
- Seafood (particularly shellfish, anchovies, and sardines)
- Beer and spirits
- High-fructose corn syrup products
- Some vegetables (asparagus, mushrooms, spinach)
2. Genetics and family history
Genetic factors play a significant role in gout development:
- About 60% of uric acid variation is determined by genetics
- Specific genes like SLC2A9 and ABCG2 affect uric acid transport and excretion
- Family history increases risk by 2-4 times
- Certain genetic disorders (Lesch-Nyhan syndrome, HPRT deficiency) cause overproduction of uric acid
3. Medical conditions
Several health conditions can increase uric acid levels:
- Obesity and metabolic syndrome
- Kidney disease or reduced kidney function
- Hypertension (high blood pressure)
- Diabetes and insulin resistance
- Hypothyroidism
- Psoriasis
- Hemolytic anemias
- Certain cancers and chemotherapy treatments
4. Medications
Certain medications can contribute to higher uric acid levels:
- Diuretics (“water pills”) like hydrochlorothiazide
- Low-dose aspirin
- Some immunosuppressants (cyclosporine, tacrolimus)
- Niacin (vitamin B3) in high doses
- Some cancer treatments
- Anti-tuberculosis drugs
5. Environmental and lifestyle factors
- Dehydration reduces uric acid excretion
- Crash dieting or fasting can temporarily raise uric acid levels
- Excessive alcohol consumption inhibits uric acid excretion
- Physical trauma to the knee can trigger a gout attack in susceptible individuals
- Stress and illness can precipitate attacks
Risk assessment for knee gout
Understanding these risk factors can help you identify your personal risk level and take appropriate preventive measures.
How to diagnose gout in the knee
If you suspect gout in your knee, it’s essential to get a proper diagnosis. A doctor will usually start with a physical exam and take your medical history, but several tests can confirm the diagnosis:
Clinical evaluation
Your doctor will examine your knee, looking for:
- Swelling, redness, and warmth
- Range of motion limitations
- Tenderness to touch
- Signs of infection or other conditions
They’ll also ask about:
- The timing and severity of your symptoms
- Previous similar episodes
- Family history of gout
- Diet and alcohol consumption
- Current medications
Diagnostic tests
Blood tests
- Serum uric acid: Measures the level of uric acid in your blood. Normal levels are typically between 3.5-7.2 mg/dL for men and 2.6-6.0 mg/dL for women. Levels above these ranges suggest hyperuricemia, a risk factor for gout.
- Inflammatory markers: Tests like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can indicate inflammation but aren’t specific to gout.
- Kidney function tests: These assess how well your kidneys are working, which affects uric acid excretion.
Joint fluid analysis
This test involves extracting fluid from the knee joint and examining it under a microscope to look for uric acid crystals. This is the most definitive test for diagnosing gout and can differentiate it from other conditions like pseudogout or infection.
Imaging tests
- X-rays: While not very useful in early gout, they can show joint damage in chronic cases or rule out other causes of knee pain.
- Ultrasound: Can detect urate crystal deposits and inflammation in and around the joint.
- Dual-energy CT scan: A specialized type of CT scan that can detect urate crystal deposits even when there are no symptoms.
- MRI: Rarely needed but can help evaluate the extent of joint damage or rule out other conditions.
Diagnostic criteria
The American College of Rheumatology uses these criteria for gout diagnosis:
- Presence of urate crystals in joint fluid
- Presence of a tophus (proven by crystal analysis)
- Fulfillment of at least 8 points from clinical, laboratory, and imaging criteria
Differential diagnosis
Your doctor will also consider other conditions that can mimic gout:
- Pseudogout (calcium pyrophosphate deposition disease)
- Septic arthritis (joint infection)
- Reactive arthritis
- Rheumatoid arthritis
- Osteoarthritis
- Knee bursitis or tendinitis
- Cellulitis (skin infection)
Accurate diagnosis is crucial for proper treatment, so don’t hesitate to seek medical attention if you suspect gout in your knee.
Effective treatment options for gout in the knee
Treating gout in the knee often involves a combination of medications, lifestyle changes, and home care to manage symptoms and prevent future flare-ups. Here are comprehensive treatment strategies:
1. Medications
For acute attacks
For long-term management and prevention
Medication timing and strategy
- Start early: Begin treatment within the first 12-24 hours of an attack for best results
- Combination therapy: Sometimes multiple medications are used together for severe attacks
- Prophylactic use: Low-dose colchicine or NSAIDs may be prescribed when starting uric acid-lowering therapy
- Treat-to-target: The goal is to maintain uric acid levels below 6 mg/dL (or below 5 mg/dL in severe cases)
2. Physical therapy and exercise
Physical therapy can be beneficial for knee gout, especially between attacks:
- Range of motion exercises: Gentle movements to maintain joint flexibility
- Strengthening exercises: Building muscles around the knee to provide better support
- Aquatic therapy: Exercising in water reduces weight-bearing stress on the knee
- Proper gait training: Learning to walk correctly to reduce stress on the knee joint
- TENS therapy: Transcutaneous electrical nerve stimulation may help with pain
3. Joint injections
For severe or persistent knee gout:
- Corticosteroid injections: Provide rapid relief by reducing inflammation directly in the joint
- Hyaluronic acid: May help improve joint lubrication and function between attacks
- Joint aspiration: Removing fluid from the knee can relieve pressure and pain
4. Lifestyle changes
Making key lifestyle adjustments can significantly reduce your risk of recurring gout attacks:
- Diet modifications: Follow a low-purine diet (detailed in the prevention section)
- Weight management: Losing weight can reduce pressure on your joints and help your body process uric acid more effectively
- Hydration: Drinking 8-10 glasses of water daily helps flush uric acid out of the body
- Alcohol limitation: Reduce or eliminate alcohol, especially beer and spirits
- Regular exercise: Low-impact activities between attacks help maintain joint health
5. Traditional and complementary remedies
Some natural approaches may help manage gout symptoms:
- Cherry juice: Contains anthocyanins that may reduce inflammation and uric acid levels
- Vitamin C: Moderate supplementation (500-1000mg daily) may help lower uric acid
- Coffee: Moderate consumption may be associated with lower uric acid levels
- Turmeric/curcumin: Has anti-inflammatory properties that may help during attacks
- Apple cider vinegar: Some find it helpful when diluted in water, though scientific evidence is limited
Treatment effectiveness timeline
Pain management for knee gout
Managing the intense pain of a gout attack in the knee requires a multi-faceted approach. Here are effective strategies for both immediate and ongoing pain relief:
Immediate pain relief strategies
1. Optimal positioning
- Elevate the knee above heart level using pillows
- Keep the knee in a slightly bent position (about 15-20 degrees)
- Avoid crossing your legs or positions that put pressure on the knee
2. Cold therapy
- Apply ice packs for 15-20 minutes every 2-3 hours
- Use a thin towel between the ice and skin to prevent frostbite
- Cold gel packs designed for joints can conform better to the knee
3. Over-the-counter pain relief
- NSAIDs like ibuprofen or naproxen (if not contraindicated)
- Acetaminophen (Tylenol) for those who cannot take NSAIDs
- Topical analgesics containing menthol or capsaicin
4. Emergency pain relief techniques
- Breathing techniques: Deep, slow breaths can help manage pain spikes
- Distraction methods: Engaging in activities that require focus
- Gentle massage of surrounding muscles (not directly on the painful area)
- Pressure point therapy on non-affected areas
Managing pain throughout a flare-up
Day 1-2: Acute phase
- Focus on rest, medication, and cold therapy
- Keep weight completely off the affected knee if possible
- Take prescribed medications exactly as directed
- Stay well-hydrated to help flush uric acid
Day 3-5: Transition phase
- Continue medications as prescribed
- Begin very gentle range of motion exercises if pain allows
- Alternate between cold therapy and lukewarm (not hot) compresses
- Gradually increase movement as tolerated
Day 6-10: Recovery phase
- Continue anti-inflammatory medications until fully recovered
- Begin more active range of motion exercises
- Apply warm compresses to improve circulation
- Gradually return to normal activities as pain permits
Pain scale management guide
Supportive devices for knee gout pain
- Knee braces: Provide stability and reduce pressure on the joint
- Crutches or canes: Reduce weight-bearing during severe attacks
- Specialized footwear: Shoes with good arch support reduce stress on the knee
- Compression sleeves: May help reduce swelling when the acute phase begins to subside
When pain requires emergency care
Seek immediate medical attention if:
- Pain is unbearable despite maximum recommended medication
- You develop a fever over 101.5°F (38.6°C) with the knee pain
- The knee becomes extremely hot, red, and swollen beyond typical gout symptoms
- You experience numbness or tingling below the knee
- You’re unable to bend or straighten your knee at all
- The pain is accompanied by shortness of breath or chest pain
Gout attack first aid: what to do during a flare-up
If you’re experiencing a gout attack in your knee, here are comprehensive steps you can take for immediate relief:
Immediate response (first 1-2 hours)
- Stop activity immediately: As soon as you feel the first signs of a gout attack, stop what you’re doing and rest the affected knee.
- Take medication: If you have prescribed medication for gout attacks (like colchicine or NSAIDs), take it immediately. The earlier you start treatment, the more effective it will be.
- Elevate your knee: Raise your leg above heart level using pillows or cushions to help reduce swelling and pain.
- Apply ice: Use ice packs on the affected area for 15-20 minutes every hour to numb the pain and reduce inflammation. Always wrap ice in a thin towel to protect your skin.
- Hydrate: Start drinking plenty of water to help flush out excess uric acid. Aim for at least 8-10 glasses throughout the day.
Next steps (2-24 hours)
- Continue medication: Follow your prescribed medication schedule strictly. Don’t skip doses even if pain begins to subside.
- Maintain elevation: Keep your knee elevated as much as possible, especially when sitting or lying down.
- Protect the joint: Avoid any pressure on the knee. Consider using a pillow or cushion to isolate the knee from accidental bumps or pressure.
- Diet modifications: Avoid all trigger foods during an attack, including:
- Red meat and organ meats
- Shellfish and oily fish
- Alcohol (especially beer)
- Sugary beverages
- High-fructose corn syrup products
- Stay hydrated: Continue drinking plenty of water and consider adding tart cherry juice, which may have anti-inflammatory properties.
Ongoing management (24-72 hours)
- Gentle movement: After 24-48 hours, if pain allows, begin very gentle range of motion exercises to prevent stiffness. Don’t force any movement that causes pain.
- Alternate ice and warmth: After the first day, you can alternate between ice therapy and warm compresses (not hot) to improve circulation and comfort.
- Monitor symptoms: Keep track of your pain levels, swelling, and any other symptoms. This information will be valuable for your healthcare provider.
- Adjust sleeping position: Use pillows to support your knee in a comfortable position while sleeping. Many find slight elevation and a pillow between the knees helpful.
When to contact a healthcare provider
- If pain is severe and doesn’t respond to your usual medications
- If you develop a fever over 101°F (38.3°C)
- If the area becomes extremely hot, red, or if redness begins to spread
- If you’re unable to move your knee at all
- If you experience new symptoms not typical of your usual gout attacks
Preventing future flare-ups
Once you’ve experienced gout in the knee, it’s essential to take steps to prevent future flare-ups. Here are comprehensive strategies for long-term management:
Dietary modifications
Foods to limit or avoid
Foods to include
- Low-fat dairy products (milk, yogurt)
- Cherries and berries (especially tart cherries)
- Citrus fruits
- Whole grains
- Plant proteins (beans, lentils in moderation)
- Nuts and seeds
- Olive oil
- Coffee (moderate consumption)
Hydration strategy
- Drink 8-10 glasses (64-80 oz) of water daily
- Increase intake during hot weather or exercise
- Consider adding lemon to water (may help alkalize urine)
- Limit or avoid alcohol, especially beer
- Reduce caffeinated beverages to moderate levels
Weight management
- Aim for gradual weight loss if overweight (1-2 pounds per week)
- Focus on sustainable dietary changes rather than crash diets
- Combine dietary changes with appropriate exercise
- Work with healthcare providers to develop a safe weight loss plan
- Set realistic goals based on your body type and health status
Exercise recommendations
Safe exercises during remission
- Swimming and water aerobics
- Cycling (stationary or road)
- Elliptical training
- Walking on even surfaces
- Tai chi and gentle yoga
- Resistance training with light weights
Exercise modifications
- Wear supportive shoes with good cushioning
- Consider knee braces during activities if needed
- Start with short sessions (10-15 minutes) and gradually increase
- Avoid high-impact activities like running or jumping
- Include proper warm-up and cool-down periods
- Stop if you experience pain beyond mild discomfort
Medication adherence
- Take prescribed uric acid-lowering medications consistently
- Don’t stop medications without consulting your doctor
- Keep “rescue” medications on hand for early intervention
- Understand potential side effects and when to report them
- Schedule regular follow-ups to monitor uric acid levels
Lifestyle factors
- Manage stress through meditation, deep breathing, or other techniques
- Establish regular sleep patterns (7-8 hours nightly)
- Avoid extreme temperature changes when possible
- Consider vitamin C supplementation (500-1000mg daily)
- Limit exposure to environmental toxins
Tracking and monitoring
- Keep a food diary to identify personal triggers
- Track uric acid levels over time
- Note any correlation between activities and flare-ups
- Monitor joint health and report changes to your doctor
- Use smartphone apps designed for gout management
Preventive supplements
- Tart cherry extract (1000-2000mg daily)
- Vitamin C (500-1000mg daily)
- Fish oil (may help with general joint health)
- Folate (may help with uric acid metabolism)
- Milk thistle (supports liver function)
Always consult with your healthcare provider before starting any supplement regimen, as some may interact with medications or have contraindications for certain health conditions.
Long-term joint health
Gout can have lasting effects on knee joint health if not properly managed. Here’s what you need to know about protecting your knee joint for the long term:
Understanding joint damage risk
Untreated or poorly managed gout can lead to:
- Tophi formation: Hard deposits of uric acid crystals that can damage cartilage and bone
- Chronic inflammation: Even between acute attacks, low-level inflammation can persist
- Cartilage degradation: Leading to joint space narrowing and osteoarthritis
- Bone erosion: Permanent changes to bone structure
- Joint deformity: In advanced cases, affecting mobility and quality of life
Relationship to other health conditions
Gout is often associated with other health issues that require comprehensive management:
- Metabolic syndrome: Including obesity, hypertension, diabetes, and high cholesterol
- Cardiovascular disease: Gout is associated with increased heart attack and stroke risk
- Kidney disease: Both a cause and consequence of hyperuricemia
- Diabetes: Often co-occurs with gout and requires coordinated management
- Osteoarthritis: Can develop alongside or as a consequence of gout
Joint protection strategies
- Maintain healthy weight: Each pound of weight loss reduces knee pressure by 4 pounds
- Use proper body mechanics: Learn correct lifting and movement techniques
- Consider supportive devices: Braces, orthotics, or walking aids when needed
- Modify your environment: Make home adaptations to reduce joint stress
- Balance activity and rest: Avoid overexertion but maintain regular movement
Rehabilitation after severe attacks
- Physical therapy: Structured programs to restore strength and range of motion
- Occupational therapy: Learning joint-sparing techniques for daily activities
- Hydrotherapy: Water-based exercises that are gentle on joints
- Gradual return to activities: Phased approach to resuming normal function
- Assistive devices: Temporary use of supports during recovery
Monitoring joint health
Regular assessment of joint health should include:
- Range of motion measurements: Tracking any limitations in movement
- Strength testing: Evaluating muscles that support the knee
- Imaging studies: Periodic X-rays or ultrasounds to assess joint status
- Functional assessments: Evaluating how well you can perform daily activities
- Pain monitoring: Tracking changes in pain patterns or intensity
When to consider advanced interventions
In cases of significant joint damage, additional treatments may be necessary:
- Viscosupplementation: Hyaluronic acid injections to improve joint lubrication
- Regenerative therapies: Such as platelet-rich plasma (PRP) injections
- Arthroscopic procedures: Minimally invasive surgery to address joint damage
- Joint replacement: In severe cases with significant functional limitation
- Specialized rehabilitation: Post-procedure recovery programs
When to see a doctor
While home care and lifestyle changes can help manage gout in the knee, it’s important to know when to seek medical attention. Here are the key situations that warrant a doctor’s visit:
Urgent situations (seek care within 24-48 hours)
- You’re experiencing your first suspected gout attack
- You have unbearable pain that doesn’t improve with over-the-counter treatments
- Your knee becomes severely swollen, red, and hot to the touch
- You develop a fever alongside knee pain and swelling
- You’re unable to put any weight on the affected leg
- You have a history of gout but the current attack seems different or worse
Emergency situations (seek immediate care)
- Extreme pain accompanied by fever over 101.5°F (38.6°C)
- Rapidly spreading redness or red streaks extending from the knee
- Numbness, tingling, or weakness below the knee
- The knee appears deformed or significantly misaligned
- You have gout along with chest pain, shortness of breath, or confusion
Follow-up care situations
- Your symptoms don’t improve after 48 hours of home treatment
- You’re having frequent gout flare-ups despite taking preventive measures
- Your joint is becoming chronically stiff or showing signs of deformity
- You’re experiencing side effects from gout medications
- You need help developing a long-term management plan
What to expect at your appointment
Be prepared to discuss:
- When your symptoms started and how they’ve progressed
- The severity and location of your pain
- Any treatments you’ve already tried
- Your typical diet and alcohol consumption
- All medications and supplements you take
- Your family history of gout or other arthritis
- Any other medical conditions you have
Your doctor may:
- Examine your knee and possibly other joints
- Order blood tests to check uric acid levels and kidney function
- Take a sample of fluid from your knee joint for analysis
- Request imaging studies like X-rays or ultrasounds
- Prescribe medications for immediate relief and long-term management
- Refer you to a rheumatologist (arthritis specialist) if needed
Questions to ask your doctor
- What can I do to prevent future gout attacks?
- Should I be on long-term medication to lower my uric acid?
- How will we know if the treatment is working?
- Are there specific foods I should avoid?
- How might gout affect my knee joint in the long term?
- How often should I have my uric acid levels checked?
- What should I do if I feel another attack coming on?
- Are there any warning signs of complications I should watch for?
FAQs
What are the 10 foods that trigger gout?
Foods high in purines can trigger gout. These include:
- Organ meats (liver, kidneys, sweetbreads)
- Game meats (venison, wild turkey)
- Shellfish (shrimp, lobster, crab, scallops)
- Oily fish (sardines, anchovies, mackerel)
- Red meat (beef, lamb, pork)
- Beer and other alcoholic beverages
- High-fructose corn syrup products
- Sugary sodas and fruit drinks
- Gravy and meat extracts
- Some vegetables (asparagus, mushrooms, spinach) in large amounts
What can I drink to flush out gout?
Drinking plenty of water is the best way to help flush out uric acid and prevent crystal formation. Aim for 8-10 glasses daily. Other beneficial drinks include:
- Tart cherry juice (4-8 oz daily)
- Coffee in moderation (may lower uric acid levels)
- Skim milk and other low-fat dairy beverages
- Green tea
- Vitamin C-rich drinks (without added sugar)
Avoid alcohol (especially beer), sugary sodas, and fruit juices with high fructose content.
What foods help clear up gout?
Certain foods are considered helpful in managing gout, such as:
- Low-fat dairy products (milk, yogurt)
- Cherries and dark berries (especially tart cherries)
- Citrus fruits (oranges, lemons)
- Vegetables (except high-purine options)
- Whole grains (oats, brown rice, quinoa)
- Plant oils (olive oil, flaxseed oil)
- Nuts and seeds in moderation
- Legumes in moderation (lentils, beans)
- Fatty fish high in omega-3s (in small portions)
Is walking good for gout in the knee?
During a gout flare-up, it’s best to rest the affected joint to avoid worsening the inflammation. However, gentle walking can be beneficial during non-flare-up periods to maintain joint health and prevent future attacks. Start with short distances on even surfaces, wear supportive shoes, and stop if pain increases. Water walking in a pool is an excellent alternative that puts less stress on the knee joint.
What is the fastest way to cure gout in the knee?
There’s no quick “cure” for gout, but taking immediate steps during an attack can help shorten its duration:
- Start prescribed medications (colchicine, NSAIDs, or corticosteroids) at the first sign of an attack
- Rest and elevate the knee above heart level
- Apply ice packs for 15-20 minutes several times daily
- Stay well-hydrated to help flush out uric acid
- Avoid trigger foods and alcohol completely during an attack
For long-term management, uric acid-lowering medications are the most effective approach.
What not to do during a gout flare-up?
During a gout attack, avoid the following to prevent worsening the pain:
- Don’t consume alcohol (especially beer)
- Avoid purine-rich foods (red meat, shellfish)
- Don’t engage in high-impact activities or exercise
- Avoid becoming dehydrated
- Don’t apply direct heat to the inflamed joint (use ice instead)
- Don’t wear tight or restrictive clothing around the knee
- Don’t stop prescribed medications without consulting your doctor
- Don’t try to “push through” the pain
How long does knee gout last?
A gout attack in the knee typically lasts 3-10 days without treatment. With proper treatment started early, the duration can often be reduced to 3-5 days. Factors affecting duration include:
- How quickly treatment is started
- The effectiveness of the medications used
- Whether this is a first attack or recurrent episode
- Your overall uric acid levels
- Presence of tophi (urate crystal deposits)
- Other health conditions you may have
Will gout go away on its own?
While a gout flare-up will eventually subside on its own, it’s highly recommended to seek treatment to reduce pain and prevent joint damage. Untreated attacks typically last longer (7-14 days) and may cause permanent joint damage. Additionally, without proper management, gout tends to become more frequent and severe over time, with shorter periods between attacks.
What is the number one food that causes gout?
Organ meats (like liver, kidneys, and sweetbreads) are often considered the top triggers for gout due to their extremely high purine content. These foods can rapidly increase uric acid levels in the bloodstream. Beer is also a significant trigger due to its double impact—it contains purines and also impairs the body’s ability to eliminate uric acid.
What else can be mistaken for gout?
Conditions that can mimic gout include:
- Pseudogout (calcium pyrophosphate deposition disease)
- Septic arthritis (joint infection)
- Reactive arthritis
- Rheumatoid arthritis
- Osteoarthritis
- Cellulitis (skin infection)
- Bursitis
- Tendinitis
- Knee injury (meniscus tear, ligament sprain)
- Lyme disease
How do I know if my knee pain is from gout?
Key indicators that knee pain may be from gout include:
- Sudden onset (often overnight)
- Intense pain that reaches maximum severity within 12-24 hours
- Redness, warmth, and swelling of the knee
- Extreme tenderness, even to light touch
- Limited range of motion due to pain and swelling
- Possible mild fever
- History of similar episodes or gout in other joints
- Improvement with gout-specific treatments
A definitive diagnosis requires medical evaluation, particularly joint fluid analysis to identify uric acid crystals.
Can stress cause gout flare-ups?
Yes, stress can trigger gout flare-ups through several mechanisms:
- Stress hormones can affect kidney function and uric acid excretion
- Stress often leads to poor dietary choices and increased alcohol consumption
- Stress can disrupt sleep patterns, which may affect uric acid metabolism
- Dehydration during stressful periods can concentrate uric acid in the blood
- Stress-related inflammation may lower the threshold for crystal formation
Stress management techniques like meditation, deep breathing, and regular exercise can be helpful components of a comprehensive gout management plan.


