This quick and easy postpartum depression quiz makes use of the Edinburgh Postnatal Depression Scale (EDPS) that was made to help health workers find out if mothers have postnatal depression.
The Edinburgh Postnatal Depression Scale is a self reported list of 10 questions designed to establish if women have postnatal depression. Items on the scale match a variety of clinical depression symptoms, and overall evaluation is established from the total score from the sum of the 10 items.1✅ JOURNAL REFERENCE
DOI: 10.1192/bjp.182.4.368
The postpartum depression quiz/scale makes use of short phrases and the mother chooses which of the 4 answers that there are to choose from are closest to how she’s been feeling in the last week.
A lot of mothers finish the postpartum depression quiz quite easily in less than 5 minutes. Data from a number of studies has proved the scale as useful for postpartum depression detection. Even so, the EPDS score should not override medical opinion. A careful medical test should be done to be sure of the result.
Postpartum depression statistics show that almost twelve percent of women had said to be moderately depressed following childbirth, and six percent had said to be very depressed following childbirth.
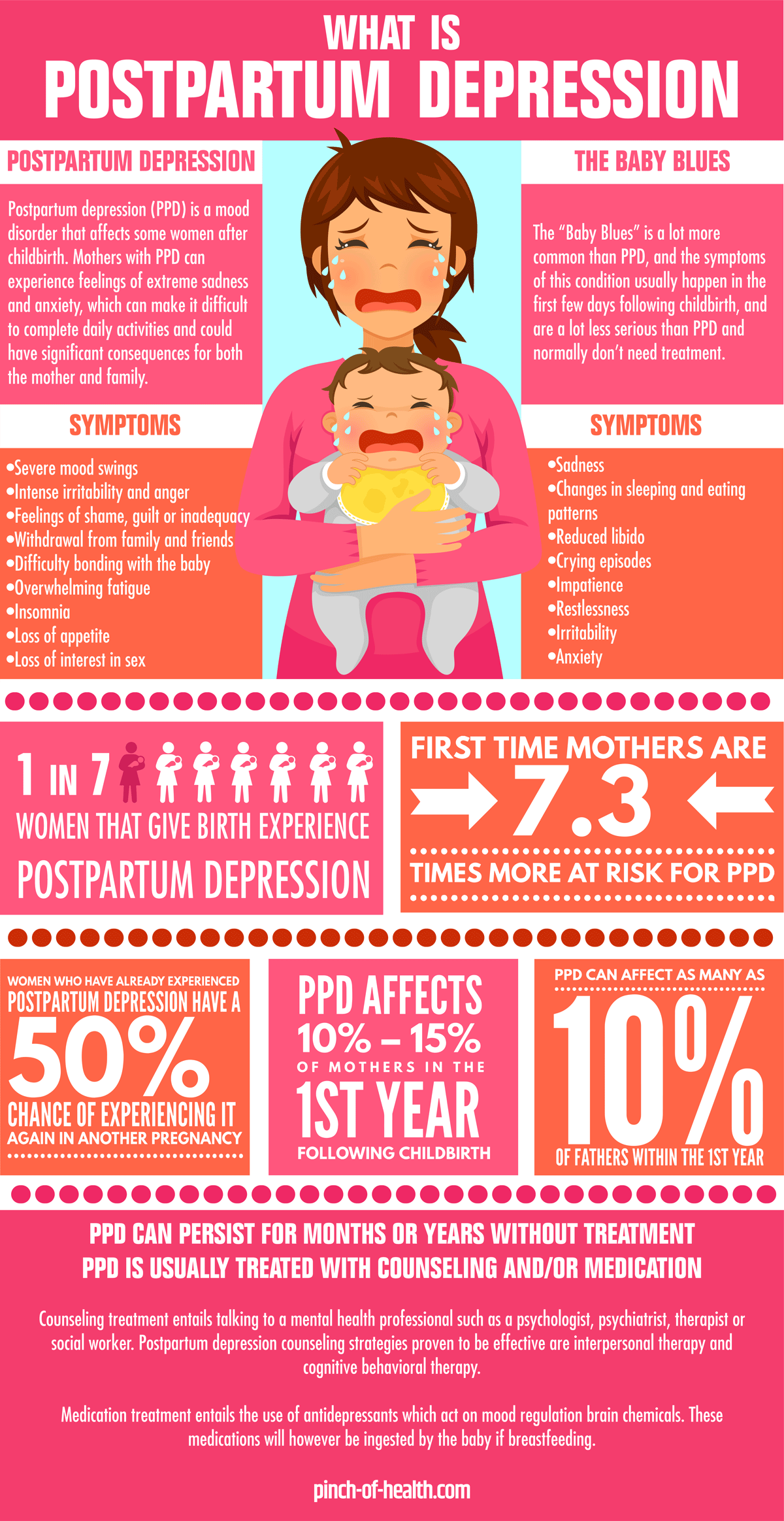
Depression in moms in their months following childbirth has come up as a major maternal and child health issue. About 1 in 7 women that give birth experience postpartum depression, which usually starts a couple of weeks following childbirth.
Postpartum depression is a severe disorder, and not the same as the ‘baby blues’, which is much milder. Symptoms can include sadness, changes in sleeping and eating patterns, reduced libido, crying episodes, irritability and anxiety.
While “baby blues” is a lot more common, the symptoms of this condition, which usually happen in the first few days following childbirth, are a lot less serious and don’t need treatment. Postpartum depression (PPD) can happen up to a year following childbirth, is a lot more serious, and needs treatment from a medical professional.
As well as directly affecting the emotional well being of moms, PPD can have an effect on marriage, the mom, infant bonding as well as behavior.
PPD can persist for months or years without treatment. PPD is usually treated with counseling and/or medication.
Counseling treatment entails talking to a mental health professional such as a psychologist, psychiatrist, therapist or social worker. Postpartum depression counseling strategies proven to be effective are interpersonal therapy and cognitive behavioral therapy.
Medication treatment entails the use of antidepressants which act on mood regulation brain chemicals. These medications will however be ingested by the baby if breastfeeding.
Postpartum depression statistics:
- First time mothers are at an increased risk for PPD. They are 7.3 times more at risk compared with women who had given birth 11 to 12 months previously.
- The 2000 postpartum depression statistics from the Centers for Disease Control and Prevention reported a 5.1% to 8.9% prevalence of severe self reported postpartum depression (SRPPD), and 48.9% to 62.3% with low to moderate depression.
- For the period of 2004 – 2005, the prevalence of SRPPD in 17 U.S. states were in the region of 11.7% to 20.4%.
- Women that suffered physical abuse while pregnant as well as women who had emotional, spouse or money related stress were more inclined than other women to have reported to be severely depressed.
- PPD affects 10% – 15% of mothers in the 1st year following childbirth.
- One study found that 1 in 5 mothers who have recently given birth an experienced postpartum mood disorders, such as depression and anxiety, don’t report their symptoms.2✅ JOURNAL REFERENCE
DOI: 10.1007/s10995-017-2361-5 - Younger mothers and others living with spouse related stress or physical abuse could be more prone to develop PPD.
- Younger women, women with lesser education, and also those who had been given Medicaid benefits for their delivery were more prone to report PDD.
- PDD was very much linked to having a lower birth weight infant and also having emotional stress while pregnant.
- PPD may also be linked to stopping breast feeding.
- The chance of PPD is higher in the age bracket of 25-45.
- A history of any other mood or mental disorder can increase the risk of postpartum depression by 30-35%.
- Low socioeconomic status and poverty have been determined to account for 25% of postpartum depression patients
Researchers have found a means of checking which women are most at risk of postnatal depression by checking for certain genetic variants.3✅ JOURNAL REFERENCE
DOI: 10.1016/j.jpsychires.2013.05.003
Existing screening guidelines for postnatal depression cases depend on making use of tools like the Postpartum Depression Quiz below, which makes use of the Edinburgh Postnatal Depression Score, yet these kinds of tests can’t determine women at risk, prior to them getting the condition.
The researchers evaluated two hundred pregnant women for postnatal depression making use of the Edinburgh Postnatal Depression Score, once on their 1st visit to the antenatal clinic, and again 2 to 8 weeks after the birth.
The women who suffered from postnatal depression had been more likely to have certain genetic variants which manage the activity of an endocrine system which is triggered as a result of stress.
The hypothalamus is a section of the human brain which monitors numerous areas of the condition of the human body’s systems and is also closely connected with the pituitary gland, which releases many different hormones in to the bloodstream which control vital body functions.
The results revealed that postnatal depression is a specific sub group of depression having a distinct genetic element meaning that some women are genetically more prone to the environmental factors that lead to depression.